You are reading Asking The Patient by Dr. Zed Zha, a doctor’s love letter that gives patients their voices back. If you enjoy it, please comment, like, share, and/or subscribe!
You are driving in a school zone under the speed limit. You see a little kid with a big backpack pushing the pedestrian signal light. You stop and wait for him to cross. He glances your way with half-asleep eyes and steps onto the zebra crossings. You chuckle.
Then a big ol’ truck speeds past you both. The little boy gets startled and hops backward onto the sidewalk.
Before you know it, you are hitting the center of your steering wheel with the heel of your hand, your arm stretched out, and your shoulder tense.
You honk.
And you honk.
You yell: “A**hole! You could have KILLED that child!”
Later at work, you recount this incident to your colleague who rages with you: “It’s not that hard to save a life. Just FOLLOW THE RULES!”
Remember this Rage.
Because that’s the Rage I felt when I received a letter of denial from the insurance company of the “prior authorization” I filled out. The prescription was for a 2-year-old’s injectable medication to treat her severe eczema.
The reason? There are “rules” I must follow called “step therapy.” (Once again, calling it “therapy” is an insult to my profession.) It goes like this: try at least two strong steroid creams before we cover a cheap non-steroidal cream; try and fail the cheap non-steroidal cream before we cover the expensive non-steroidal cream; once you try and fail the expensive non-steroidal cream, we will THINK ABOUT covering the injectable medicine.
It’s THAT simple! Just follow these rules and save a life!
Except, this is what life looks like now:
My little patient had only been alive for 24 months but hadn’t slept for 18 of those months, including last night, the night before, and the night before that…because she stayed up all night crying and scratching her skin raw.
Her parents stayed up all night, too, trying to soothe her and hoping she would exhaust herself to sleep.
For 18 months, they went to the last doctor after the doctor before the last doctor after the doctor before that doctor asking for help. And all they did was give her more creams.
The creams, damn the creams!
They were always too small of a tube, or the same cream as the last cream, or only prescribed for 14 days with no refills…
Oh and … the doctors said:
“Don’t feed the baby this,” “Don’t feed the baby that,” “Something is wrong with your breastmilk,” “Play some calming music at night,” “Avoid baths,” “It’s allergies,” “It’s not allergies,” and what did the other doctor say again she couldn’t remember because SHE HADN’T SLEPT FOR 18 MONTHS?
“BE A BETTER MOTHER!” They implied.
Finally, the sleepless, miserable mother brought the sleepless, miserable child who was more rash than human into my office, praying I could do something. And she did this throughout the visit (and all day and all night):
Trigger Warning: this video involves imagery and sounds that depict a scratching child, which can provoke uncomfortable feelings. You don’t have to play it. If you do, know that I’m with you.🩵
Disclaimer 1: The above video is an example of a baby suffering from eczema, not “the patient” described in this story. It is non-patient-identifying but shared with permission nonetheless.
And what did I do?
I prescribed more creams because we had to follow “the steps” required by insurance.
Remember that Rage?
That day, I saw that Rage from my patient’s mother. I received that Rage. I felt that Rage reaching inside my chest and squeezing my heart.
And guess what? I deserved that Rage.
This is what I wrote one day after the visit:
I tried to explain why I had to do this and promised I would get her better. I just needed more time. Just a few more months to complete “the steps.” To a mother who didn’t even have one more month in her, my empty, muffled words might as well come from underwater.
When I hugged her (with her permission), it felt like I was hugging the skeleton of a person.
Note: Prior Authorization is a process required by the “payors” (insurance companies) to have a medication approved for payment before patients receive it. It’s a cost-cutting strategy. It’s a well-known barrier to care. Prior authorization leads to a delay in care in 94% of cases, including 69% of cancer patients. It also leads to a 78% chance a treatment option would be abandoned. Fighting the denials is a tedious task, time-consuming, frustrating, and a total guessing game. And when we lose the fight, patients think it’s the doctors who don’t want to prescribe — it compromises the therapeutic relationship and is a way to pit patients against physicians. Not to mention, rejecting a physician’s prescription is practicing medicine without a license (fraudulent), dictating a patient’s care from outside of the exam room (unethical), and failing to fulfill the contract to pay for the care a patient needs (illegal).
After that visit, I wrote the newsletter My Unspoken Words.
And surprisingly, it got the attention of the company that makes this injectable medication. Soon after, a team reached out to offer it for free! Due to regulations at my work, I contacted a physician at a free clinic to help me receive it. Even though I had never met this doctor before, she graciously agreed to help.
Meanwhile, a clinician colleague and a pharmacist at my work helped me brainstorm ways to get insurance to “allow” me to skip the “steps.” A therapist colleague offered to reach out to the family for support while we waited. My medical assistant (who is a mother herself) kept calling to check on the mother.
A few weeks later, I had another clinic visit with the child. This time, the father came, too. “I will pay for the medicine! I HAVE the money!” He pleaded with tears in his eyes.
They didn’t have money. Working with a marginalized immigrant community, I knew that no one had the kind of money to sustain a medicine that cost thousands of dollars a month.
I will never forget the look the tired father wore on his face — he needed to be angry but he didn’t know whom at; he wanted to cry but he had to be “the strong one” as his wife hid her face in tear-stained sleeves; he heard my promises to help and my explanations of why not now but it was too late and too unbelievable.
He couldn’t believe that the world could be so cruel. That god could be so cruel. That these English-speaking, white coat-wearing people with fancy diplomas could be so cruel.
He didn’t say it but his eyes did: “YOU would have NEVER done this to us if we weren’t poor, if we spoke English, if we had better status… So, here, take your stupid money and help our child!”
That day at lunch, I called my contact from the drug company and pleaded for a faster delivery of the free samples. I didn’t care if he had to hand-deliver it to us. I didn’t care if I needed to drive somewhere to get it.
“We will get it to you, Doc.” He told me after I described what I saw in clinic.
Call me naive but, I’d like to believe that, at that moment, I wasn’t a doctor from whom drug companies couldn’t make big bucks, and he didn’t represent any corporation. We were just two humans who felt at our core that we couldn’t fail a child one more day.
That very afternoon the samples arrived at the free clinic. I was elated. Everyone involved was. I couldn’t wait to tell the family about it. But it was late during the day and they didn’t answer my call. “We will call them again first thing tomorrow morning,” my medical assistant reassured me.
“How was your day?” My mother asked me at dinner.
“It was…” I had just picked up some rice with my chopsticks. But suddenly I couldn’t take a bite. I swallowed the lump in my throat as my eyes watered.
“Sweetie, we don’t have to talk about it if you don’t want to.” My mother said gently.
That night, I dreamed that I forgot to call my patient’s family the next day which somehow cost them the chance at the medication entirely. When I woke up, it was only 3 am. At first, I was frustrated that I couldn’t fall back to sleep. Then I remembered that however many hours of sleep I had already had — was exactly the number of hours my patient and her family didn’t.
I got out of bed and wished the morning sun to rise.
I’m happy to report that we got my patient the medicine she needed — not just the free samples, but we also got it approved through insurance (after many fights — I won’t bore you with the details, but if you are curious, here is an example and here is an audacious request from them that got me PO)!
When my patient’s mother brought her in to learn to administer the medicine from a nurse, I was working in a different location. Suddenly, I received five messages from different people at work updating me on how it went. Everyone sounded so excited.
“Please give the mom a hug for me! 🥹🥹🥹” I texted them back.
That afternoon, five shoulder-squeezing, body-enveloping, spirit-lifting, and life-infusing, whole-hearted, high-quality hugs were given to a mother who needed them more than anything.
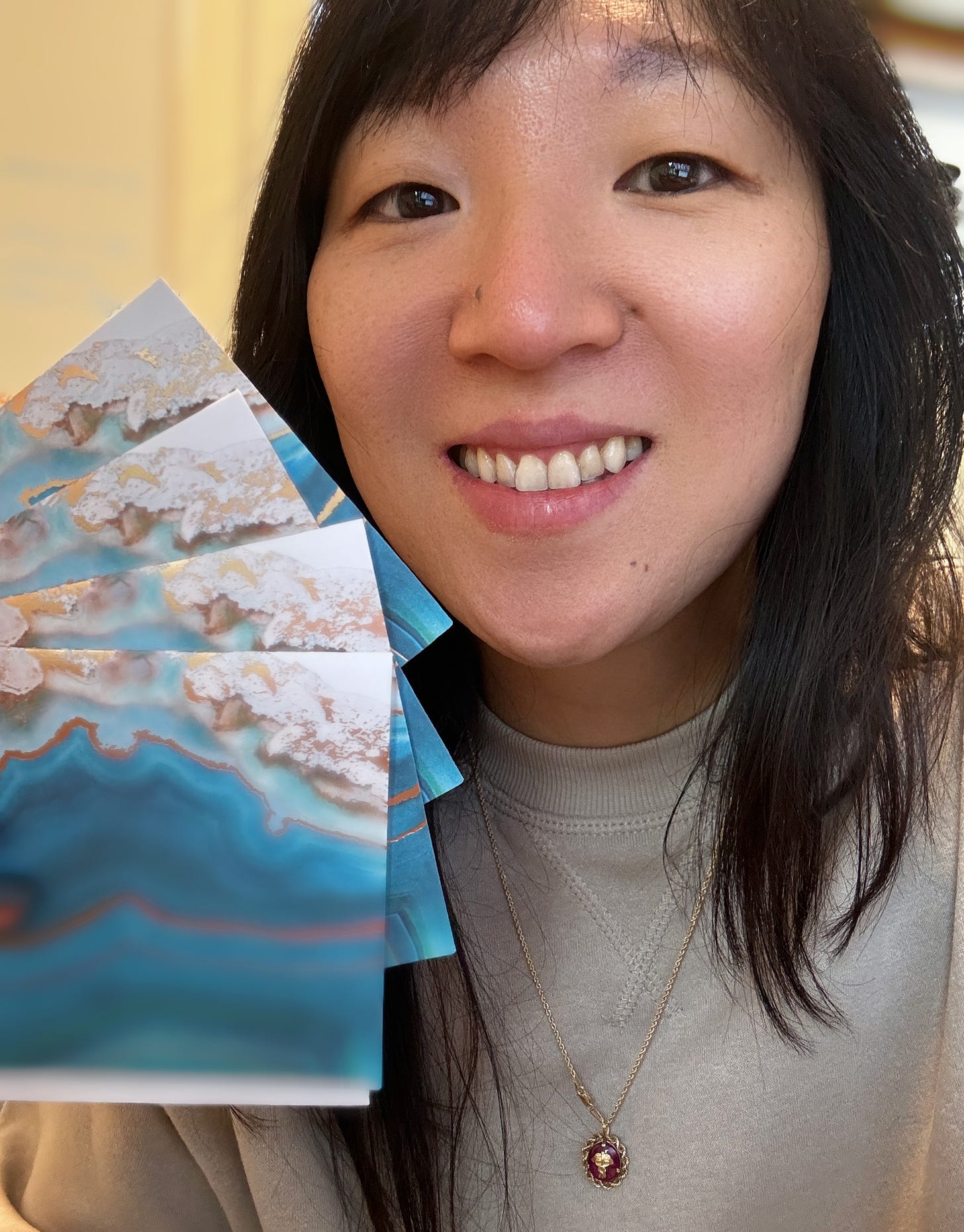
PS: I thought I’d be writing a Rageful letter to the insurance company, which would have been a MASSIVE waste of my life. Instead, I am so filled with gratitude that I decided to write thank-you notes to everyone mentioned above who helped me save a life (and helped me learn how to do it better next time)! (But guess who ain’t gettin’ one??🤣🤣😡)






Thank you so much for writing. So many of us in healthcare want to share stories so the world sees just how uncaring the American healthcare system is...... but we're soooo exhausted just trying to show up for our patients. (no excuses, just truth) I am a RN in a short-staffed busy city hospital; I see the consequences of delayed care every single day. And when I worked in a community clinic, the staff fought like you are for every inch we could wrestle from the insurance companies. Thank you again. When I catch my breath, I will be following up on the outlines I've started as letters to the editors...
Thank you for advocating for this child. As a heath care provider, I feel that rage, too. Health care is so very challenging to provide, because of these rules. Thank you for maintaining your compassion. Hugs to YOU!